02
“Hey! Can you help dress this wound?”
“Emergency patient incoming!”
It was my first day at the university hospital,
a place where emergency patients and regular patients alike flooded the halls.
Especially in thoracic surgery—every operation was high-stakes,
the kind of cases most med students dreaded.
I was the only first-year resident in this department.
Which meant I had to move faster, handle more,
even though it was just my first day.
“What brings you in today?”
“Lately I’ve had sudden shortness of breath, my heart races, and I think I’ve had a bit of a fever…”
“Can I take your hand for a moment?”
As the patient listed their symptoms,
I noticed a bluish tint on their lips.
It immediately made me suspect cyanosis,
so I asked for their hand.
Sure enough, even their fingernails had turned blue.
Cyanosis: A bluish discoloration of the skin and mucous membranes,
often suggesting cardiac or pulmonary disease.
“You’re showing signs of cyanosis.
That could mean a heart or lung issue.”
“We’ll need to do an EKG and a chest CT scan.”
“We’ll get those done and go over the results with you afterward,
so try not to worry. We’ll take good care of you.”
After seeing several patients,
I used a short break to check on the ICU.
More than half our department’s cases were emergencies or critical care,
so the ICU was packed.
I was checking on patient charts when a nurse urgently called out to me.
“This patient has a pneumothorax. Can you insert a chest tube?”
“Sorry, a chest tube insertion?”
“Yes, it’s an emergency.”
“…We should start with a chest X-ray.”
Chest tube insertion: A procedure to drain air, fluid, or blood from the chest cavity.
Chest X-ray: An imaging test of the thorax to evaluate heart and lung conditions.
Chest tube insertion was typically left to second-year residents or above,
unless under direct supervision from an attending.
But I was a first-year,
on my first shift,
with my first emergency patient,
and this would be my first chest tube insertion.
I had watched countless videos—
but doing it for real was different.
Still, the patient was critical.
There was no time to wait.
Though not a major surgery,
this procedure—done under local anesthesia—should still be performed with a supervising physician.
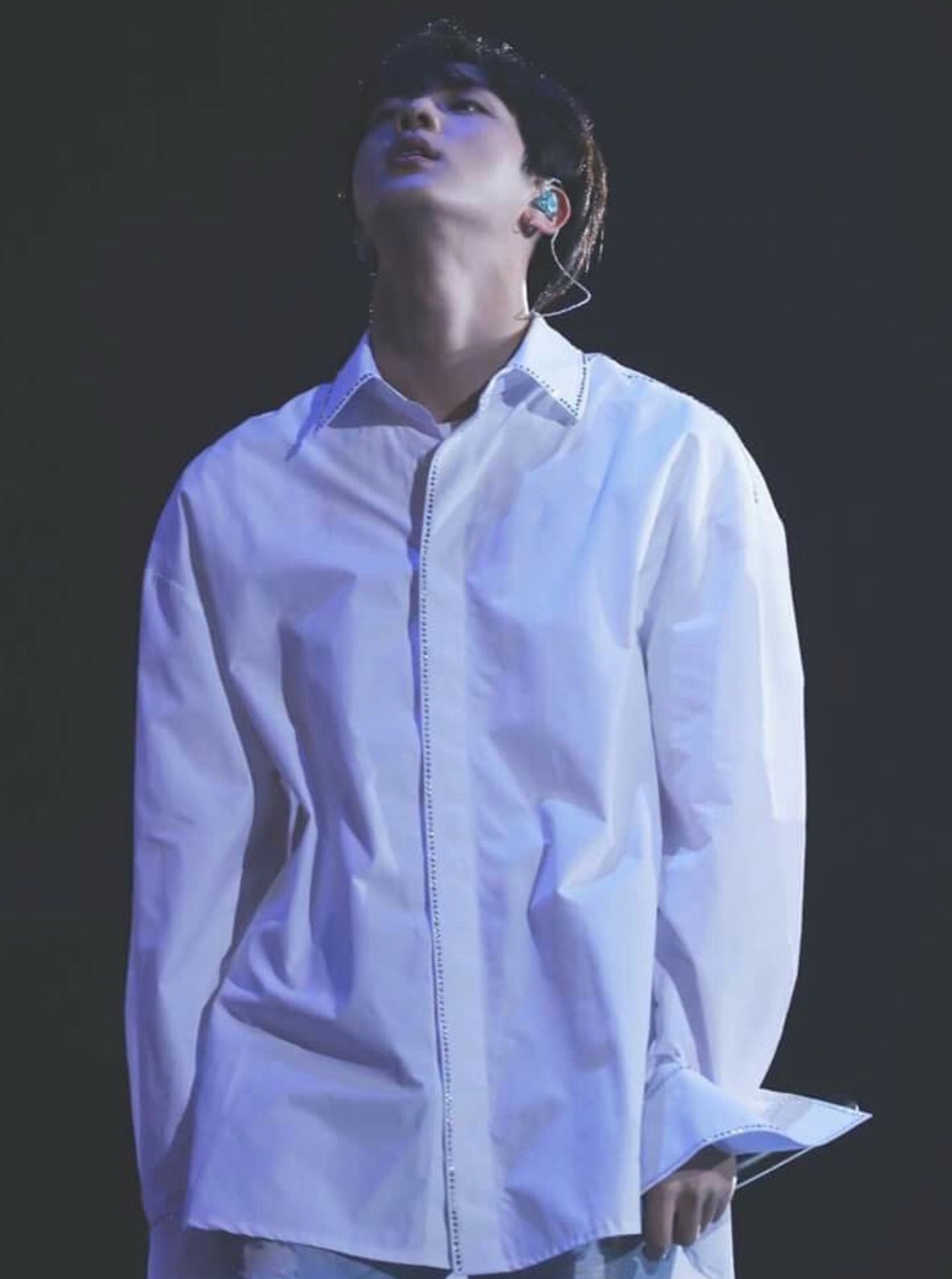
But Professor Kim Seokjin wasn’t around.
And I had to act.
Local anesthesia: A method that numbs a specific area of the body while the patient remains conscious.
So I did it.
I inserted the chest tube.
It seemed to go well.
No complications, stable vitals.
But whether it went well or not,
a first-year resident performing that alone was a serious protocol breach.
And of course,
news of it reached Professor Kim.
Soon, a voice like a blade cut through the air.
“Yoon Seo-ah.
Come to my office.
Right now.”
